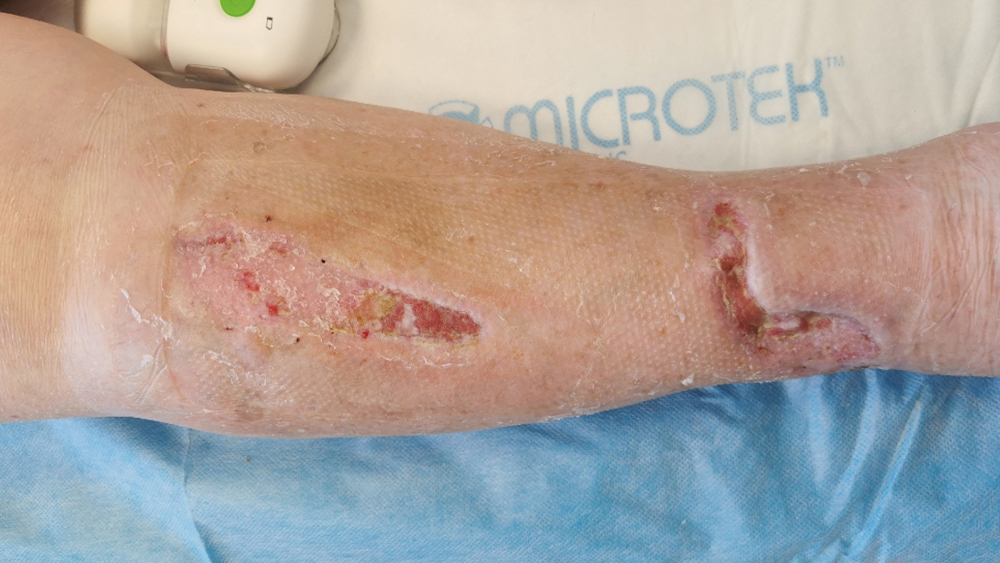
Case Study: Dehisced leg trauma wound, skin grafts
The Avance® Solo Negative Pressure Wound Therapy System is indicated for patients who would benefit from wound management via the application of negative pressure, particularly as the device may promote wound healing through the removal of exudate and infectious material.
Photographs and case notes kindly supplied by Sanna Kouhia, Vascular Surgeon; Tuula Eskelinen, Wound Care Nurse; Arja Korhonen, Wound Care Nurse, the surgery outpatient clinic / wound outpatient clinic, Kainuu Central Hospital, Kajaani, Finland
Wound history
A 72-year-old female with a current treatment for hypertension, peripheral vascular disease and chronic pulmonary disease, presented with a dehisced leg wound.
44 days prior to the baseline visit, the patient had fallen, wounding her right ankle, and in addition, causing a small contusion in the right leg proximally and anteriorly.
A large haematoma developed in the area of the bruise and the skin went into necrosis. The ankle wound was primarily sutured, however, the wound dehisced. Due to the negative progression of both wounds, a revision was performed and a traditional NPWT system was applied. Later, the wounds were found to be still covered with fibrin. There was larval treatment between the wound care visits, during which time the NPWT was stopped.
Treatment regime
44 days after the trauma, an additional wound revision was performed and skin grafts were applied.
A portable negative pressure wound therapy system was applied successfully under a compression bandage and a support stocking. One NPWT dressing, size 15 x 30 cm, covered both wounds.
Outcome
Review at baseline showed two wounds with a size of 10 cm x 3 cm and 12 cm x 4 cm, respectively and both with a depth of 1 cm. The majority of the wound areas were granulated (90%) and there was slough present (10%), but no necrotic tissue. Exudate levels were low and clear/serous in appearance.
12 days after the first visit, the wounds had progressed, with 80% of the wounds epithelialised and 20% actively granulating. The level of exudate in the canister was low, however, moderate exudate levels within the wound were viscous, and brown/bloody in appearance.
At follow up visit No 3 (30 days), the wound on the ankle had decreased in size to 0.4 cm x 1 cm with a depth of 0.2 cm and with 90% of the surface epithelialised, and 10% granulated. The second wound was fully healed.
A moderate amount of exudate was still brown/bloody and viscous in appearance.
44 days (88 days after the trauma) after the first visit, both wounds were fully healed.
There were no signs of infection in any of the wounds for the duration of the treatment duration and no antibiotics were administered.
The periwound appeared healthy throughout the duration of treatment and application of a wound filler was not necessary.
No additional dressing changes occurred outside of the planned follow-up visits.
Sharp debridement was performed at each follow-up visit, except during visit 4 (44 days after the baseline).
The patient reported there was no pain before or during dressing removal.
Performance
All performance aspects of the device were perceived to be ‘Very good’ including, the suitability of the size and shape of the dressing. The dressing size of 15x30 cm conformed well on the tibia and covered both skin grafts.
Exudate management was very satisfactory, especially since one dressing was used to cover both wounds.
The overall impression of the device was very good as this was a complicated trauma to treat and the skin graft healed quickly following revision and grafting. The device had also been easy and effortless to use.
Patient experience
The patient was satisfied with the treatment throughout the treatment period, perceiving it as effortless and painless. She was very pleased with the need for only a few dressing changes and easy management of the device during treatment.